September 11, 2025

The article highlights the critical role of continuous measurement strategies in maximizing patient care within healthcare settings. Continuous measurement facilitates real-time data collection on vital metrics, which is essential for the early detection of patient deterioration. This capability enables informed decision-making, ultimately leading to improved patient outcomes and enhanced operational efficiency. By implementing these strategies, healthcare providers can significantly elevate the quality of care they deliver.
The constantly evolving healthcare landscape demands innovative strategies to enhance patient care, with continuous measurement emerging as a pivotal approach. This methodology not only facilitates real-time tracking of vital metrics but also empowers healthcare providers to make informed decisions that can significantly improve patient outcomes. Yet, a pressing challenge remains: how can organizations effectively implement continuous measurement practices to fully realize its benefits while navigating compliance and regulatory hurdles?
Constant assessment in medical settings serves as a critical framework for continuous measurement, enabling the structured and persistent gathering of information related to individual treatment procedures and results. This method empowers healthcare providers to perform continuous measurement of essential metrics—such as vital signs, treatment responses, and client satisfaction—in real-time.
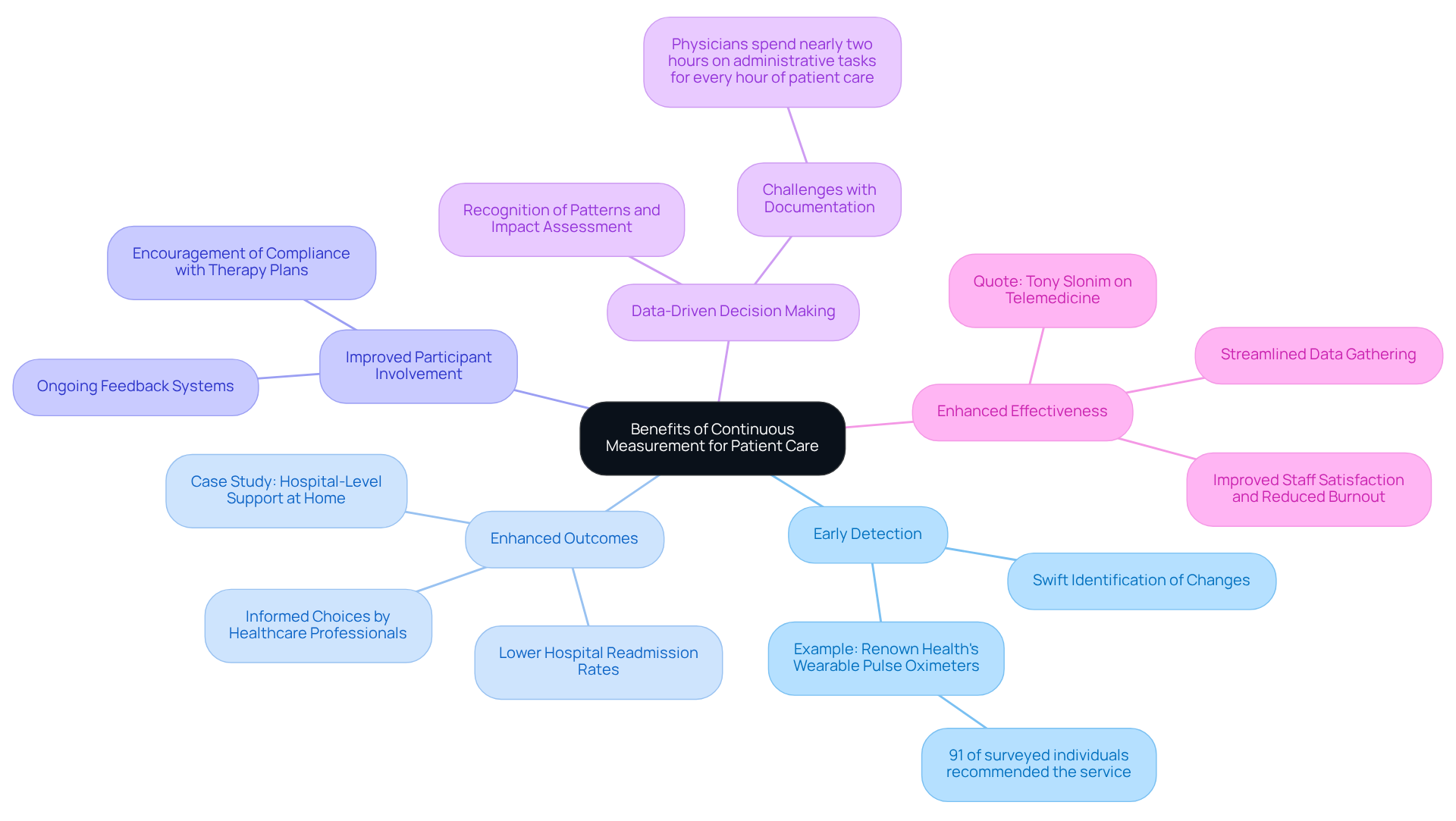
By utilizing continuous measurement, organizations can swiftly identify trends, detect anomalies, and make informed decisions that enhance care for individuals. Consider this: continuous measurement of vital signs can alert clinicians to early signs of deterioration, facilitating prompt interventions that significantly improve outcomes. This proactive approach starkly contrasts with conventional sporadic assessment, which often overlooks crucial changes in an individual's condition due to its irregularity, highlighting the .
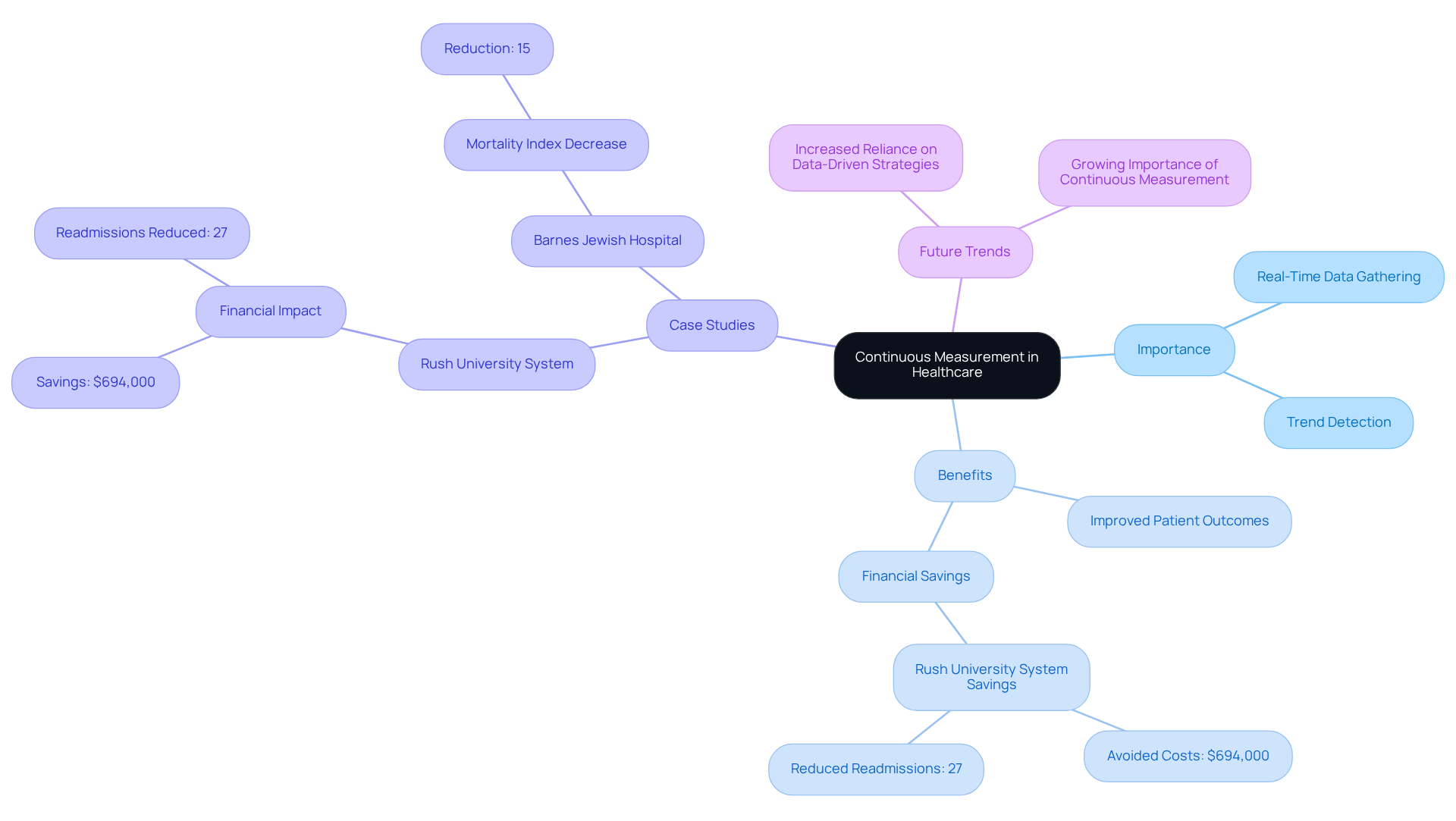
Continuous measurement is indispensable for quality enhancement efforts, as it provides the necessary data to evaluate service effectiveness and instigate timely modifications. Looking ahead to 2025, the importance of continuous measurement will only grow, as healthcare systems increasingly rely on data-driven strategies to elevate care and outcomes.
Notably, the Rush University System for Health's reduction in readmissions, which saved an estimated $694,000 in potential costs, underscores the financial benefits of ongoing assessment. Additionally, Barnes Jewish Hospital's enhancement initiative, resulting in a 15% decrease in the mortality index for ED patients, highlights the tangible impact of ongoing assessment on patient outcomes.
As medical leaders emphasize the necessity of continuous measurement, expert testimonies further validate its role in enhancing service quality and operational efficiency.
To implement effective continuous measurement strategies, healthcare organizations should consider the following steps:
By implementing these strategies, medical organizations can establish a strong framework for ongoing assessment that improves individual support and results. The focus on technology and participant engagement reflects the current initiatives by CMS to enhance healthcare quality and equity.

Continuous measurement significantly enhances patient care through several key benefits:
In conclusion, incorporating continuous measurement into medical practices not only enhances care for individuals but also contributes to creating a more efficient and effective medical system.
To ensure compliance and regulatory alignment in continuous measurement practices, healthcare organizations must prioritize the following actions:
By prioritizing compliance and regulatory alignment, healthcare organizations can enhance their practices of continuous measurement while safeguarding patient rights and maintaining high standards of care. Additionally, organizations should be vigilant about common pitfalls, such as the tendency to overlook the need for annual training or the risks of inadequate audits, which can compromise their compliance efforts.

Incorporating continuous measurement strategies in healthcare signifies a transformative shift towards more effective patient care. This approach underscores the critical role of real-time data collection and analysis, enabling healthcare providers to respond swiftly to fluctuations in patient conditions. By prioritizing continuous assessment, organizations can significantly enhance treatment outcomes, elevate patient satisfaction, and cultivate a culture of proactive care.
The article delineates several compelling arguments advocating for the implementation of continuous measurement. These include:
By harnessing technology and weaving measurement into daily operations, healthcare organizations can streamline processes and concentrate on delivering high-quality care. Moreover, adherence to regulatory standards guarantees that these practices are not only effective but also ethically sound and respectful of patient privacy.
Ultimately, the adoption of continuous measurement is vital for advancing healthcare quality and efficiency. As the healthcare landscape evolves, embracing these innovative strategies will be essential for organizations striving to improve patient outcomes and sustain a competitive edge. Engaging in continuous measurement not only elevates individual care but also contributes to a more robust and responsive healthcare system, highlighting the imperative for all healthcare stakeholders to prioritize these practices.
What is continuous measurement in healthcare?
Continuous measurement in healthcare refers to the constant assessment of individual treatment procedures and results, enabling the structured and persistent gathering of information related to vital signs, treatment responses, and client satisfaction in real-time.
How does continuous measurement benefit healthcare providers?
It allows healthcare providers to swiftly identify trends, detect anomalies, and make informed decisions that enhance care for individuals, leading to improved patient outcomes.
Why is continuous measurement important for patient care?
Continuous measurement is important because it can alert clinicians to early signs of deterioration, facilitating prompt interventions that significantly improve outcomes, unlike sporadic assessments that may overlook crucial changes in a patient's condition.
What role does continuous measurement play in quality enhancement efforts?
Continuous measurement provides the necessary data to evaluate service effectiveness and instigate timely modifications, making it indispensable for quality enhancement in healthcare.
How is the significance of continuous measurement expected to change by 2025?
By 2025, the importance of continuous measurement is expected to grow as healthcare systems increasingly rely on data-driven strategies to elevate care and outcomes.
Can you provide examples of the financial and clinical impacts of continuous measurement?
The Rush University System for Health saved an estimated $694,000 in potential costs by reducing readmissions through continuous measurement. Additionally, Barnes Jewish Hospital achieved a 15% decrease in the mortality index for ED patients, demonstrating the tangible impact of ongoing assessment on patient outcomes.
What do medical leaders say about the necessity of continuous measurement?
Medical leaders emphasize the necessity of continuous measurement, and expert testimonies validate its role in enhancing service quality and operational efficiency.
Our expert recruitment strategies and AI-driven sourcing ensure that you receive top-notch candidates quickly, without compromising on quality. Whether you’re looking for BCBAs, Clinical Directors, or RBTs, we’ve got you covered.