May 30, 2025

Behavior significantly impacts healthcare outcomes and patient care, influencing treatment adherence, engagement, and overall health status. Engaged patients are more likely to follow medical advice. Addressing psychological and social factors can further enhance compliance and wellness outcomes. This ultimately leads to improved healthcare results. Consider how these insights might apply to your own practices and the potential benefits of fostering patient engagement.
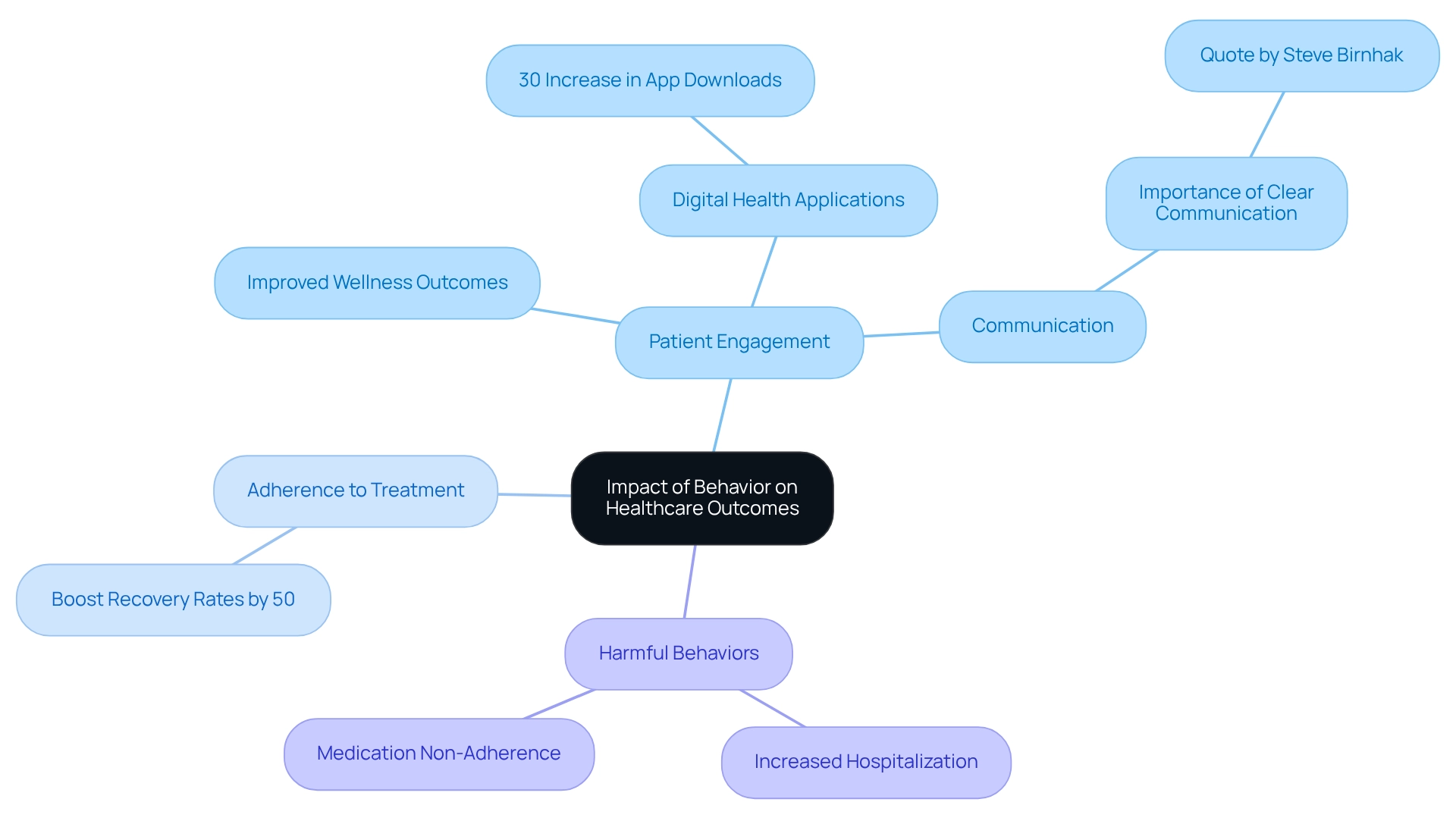
In the realm of healthcare, the significance of behavior cannot be overstated. Research consistently highlights how patient engagement, adherence to treatment plans, and lifestyle choices are pivotal in determining health outcomes. Engaged patients are more likely to follow medical advice and attend necessary appointments, leading to improved recovery rates and overall well-being.
But what happens when patients avoid care or neglect their prescriptions? Negative behaviors can exacerbate health issues, resulting in increased hospitalizations and soaring costs.
As the healthcare landscape evolves, understanding the psychological and social influences on patient behavior becomes essential for developing effective interventions. By integrating behavior analysis into healthcare practices, providers can enhance patient care and operational efficiency, paving the way for a healthier future.
Conduct significantly influences medical outcomes, with research consistently demonstrating that involvement, adherence to treatment strategies, and lifestyle choices are essential components of recovery rates and overall health. Individuals who are engaged in their care are markedly more likely to follow medical advice, attend follow-up appointments, and comply with prescribed therapies, collectively leading to improved wellness outcomes.
In contrast, harmful behavior or behaviour such as medication non-adherence and avoidance of medical treatment can worsen health conditions, resulting in increased hospitalization rates and escalating medical costs. A study in the Journal of Health Psychology underscores that individuals who actively participate in their care decisions report superior wellness outcomes, highlighting the pivotal role of behaviors within healthcare settings.
Moreover, integrating behavioral wellness strategies into primary care has shown significant promise in enhancing outcomes by addressing the psychological and social factors that influence behavior related to wellness. For instance, the COVID-19 pandemic has accelerated the adoption of digital health applications, evidenced by a 30% increase in medical app downloads, reflecting a shift towards more engaged care for individuals.
Data indicates that adherence to treatment plans can boost recovery rates by as much as 50%, underscoring the importance of fostering positive behavior among patients. With the demand for Board Certified Behavior Analysts (BCBAs) projected to increase by 25% by 2026, the focus on behavior or behaviour in medical environments will be increasingly crucial for developing effective treatment strategies and improving client outcomes.
Transparent communication between patients and healthcare providers is vital, as emphasized by Steve Birnhak, COO/Co-Founder of Ready Set Recover. Furthermore, with over 470,000 clients utilizing Updox daily for interaction and communication, the significance of engagement tools in enhancing medical outcomes is undeniable. The Updox database, which contains patient engagement data for 150 million individuals, further substantiates the claims regarding the impact of patient engagement on health outcomes.
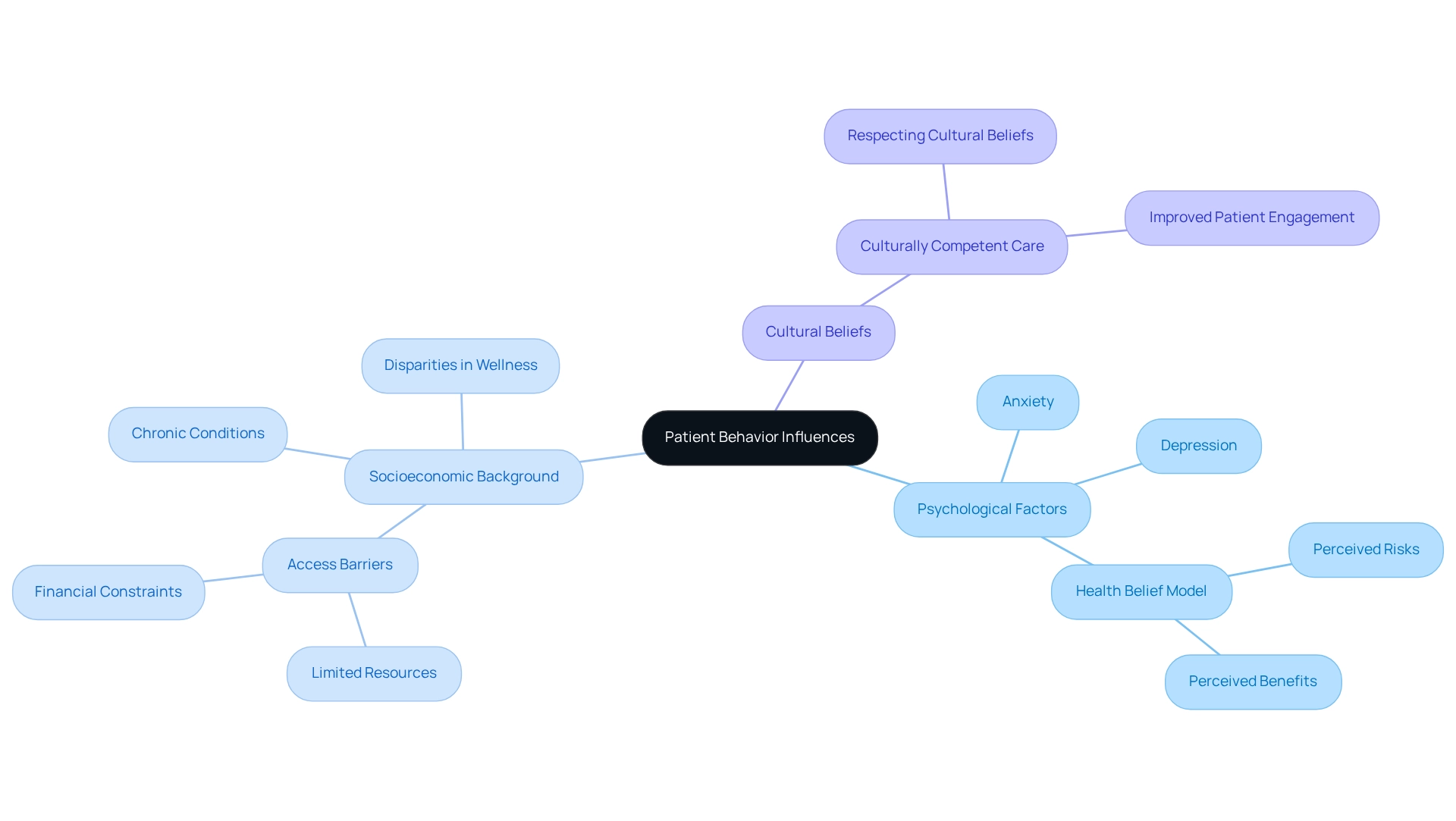
The behavior of patients is significantly influenced by a blend of psychological and social elements, encompassing mental well-being, socioeconomic background, and cultural beliefs. Individuals from lower socioeconomic backgrounds often encounter substantial barriers to healthcare access, such as limited resources and financial constraints, which can lead to poorer wellness outcomes. Studies reveal that socioeconomic disparities can cause notable variations in well-being status, with affected individuals experiencing higher rates of chronic conditions and lower overall wellness ratings. Notably, research indicates that among older individuals, Whites and Hispanics frequently face the most pronounced socioeconomic disparities in respondent-rated well-being.
Psychological factors, particularly anxiety and depression, can further complicate an individual's capacity to engage effectively with healthcare providers. The Health Belief Model illustrates how an individual's perceptions of risks and the perceived benefits of taking action significantly influence their health behavior. As Yeonwoo Kim notes, "The results indicate that different socioeconomic patterns in the two health indicators are possibly due to different underlying mechanisms of respondent-rated health and obesity." This model underscores the importance of understanding these psychological influences on behavior to tailor interventions that address the specific challenges faced by individuals.
Culturally competent care is essential for enhancing individual engagement. By respecting and integrating individuals' cultural beliefs into their care strategies, providers can foster compliance and involvement, ultimately leading to improved wellness outcomes and positive health behavior. For example, case studies have shown that when healthcare providers employ culturally sensitive approaches, patients are more likely to participate actively in their treatment, resulting in better wellness metrics.
Moreover, addressing socioeconomic barriers is vital for effective healthcare behaviour. The case study titled "Health Data Collection and COVID-19" explores the implications of medical data collected during the pandemic, suggesting that future research will benefit from baseline statistics on socioeconomic disparities in wellness before, during, and after the pandemic. Expert perspectives emphasize the need for targeted public welfare initiatives that consider the unique challenges faced by socioeconomically disadvantaged communities. By focusing on these factors, healthcare systems can work to reduce disparities in wellness and enhance overall care for individuals.
In conclusion, understanding the psychological and social factors that influence individual behavior or behaviour is crucial for healthcare practitioners. By integrating these insights into their practice, they can develop more effective strategies to engage individuals and improve health outcomes.
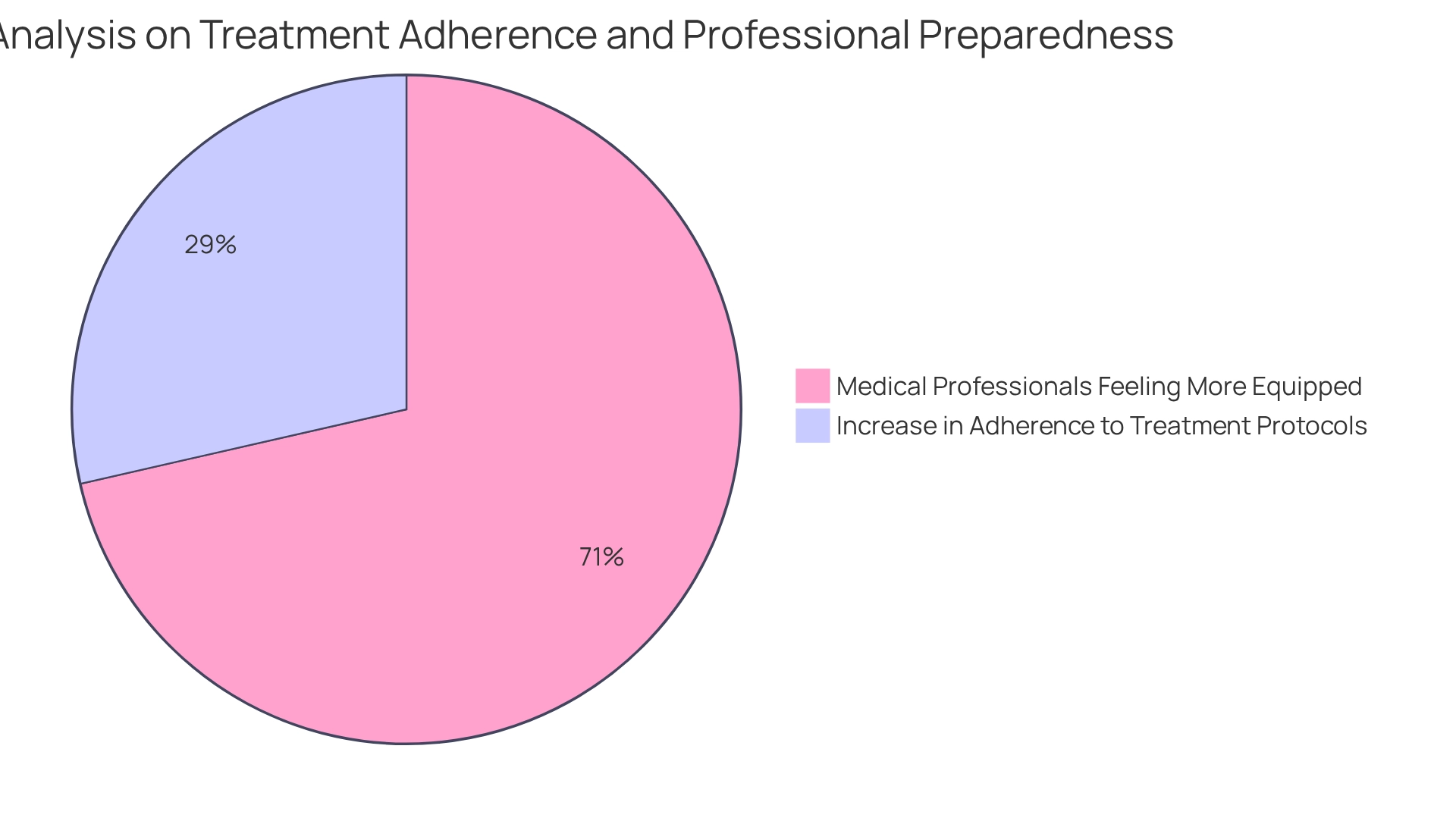
The incorporation of conduct analysis within medical environments is crucial for enhancing client care and operational efficiency. Did you know that the implementation of analysis strategies in clinical settings can lead to a significant 30% increase in adherence to treatment protocols? Methods such as functional assessments and modification strategies empower healthcare providers to identify and rectify actions that adversely affect outcomes for individuals receiving care. For instance, analysts can craft tailored strategies aimed at improving medication compliance among individuals with chronic conditions.
A study utilizing a retrospective, observational design examined data with R, version 3.8.0, confirming the substantial impact of these strategies. Training medical personnel in behavior analysis principles not only fosters a supportive environment but also promotes positive behavior or behaviours in clients. Furthermore, a survey indicated that 75% of medical professionals engaged in cross-disciplinary training felt more equipped to handle complex client requirements. Operational efficiency is further enhanced by optimizing workflows and minimizing redundancies through behavior-based management practices. This approach not only elevates patient satisfaction but also improves resource distribution, ultimately leading to superior service delivery. Ongoing professional development in ABA therapy is essential to remain abreast of the latest research and techniques, ensuring that healthcare providers can effectively implement behavior analysis practices.
The influence of behavior on healthcare outcomes is profound and multifaceted. Engaging patients in their care leads to significantly improved adherence to treatment plans and better overall health. As evidenced by various studies, patients who take an active role in their healthcare decisions tend to experience superior outcomes, while negative behaviors can exacerbate health issues and increase costs. The rise of digital health tools further underscores the importance of fostering patient engagement, reflecting a shift that can enhance recovery rates and reduce hospitalizations.
Understanding the psychological and social factors that shape patient behavior is equally critical. Socioeconomic disparities and cultural beliefs can create barriers to effective healthcare, leading to poorer health outcomes for certain populations. By employing culturally competent care and tailored interventions, healthcare providers can address these challenges, ultimately improving patient engagement and health metrics. This highlights the need for a comprehensive approach that considers both the individual and systemic factors influencing health behaviors.
The implementation of behavior analysis in healthcare settings serves as a powerful strategy for enhancing patient care and operational efficiency. By utilizing behavior modification techniques and training staff in these principles, healthcare organizations can create an environment that promotes positive patient behaviors. This not only leads to improved adherence but also optimizes resources and enhances overall healthcare delivery. As the focus on behavior in healthcare continues to grow, it becomes increasingly clear that integrating these insights into practice is essential for achieving better health outcomes and fostering a healthier future for all.
How does patient conduct influence medical outcomes?
Patient conduct significantly influences medical outcomes, as research shows that involvement in care, adherence to treatment strategies, and lifestyle choices are essential for recovery rates and overall health.
What are the consequences of harmful behaviors in healthcare?
Harmful behaviors, such as medication non-adherence and avoidance of medical treatment, can worsen health conditions, leading to increased hospitalization rates and higher medical costs.
What evidence supports the importance of patient engagement in healthcare?
A study in the Journal of Health Psychology indicates that individuals who actively participate in their care decisions report better wellness outcomes, highlighting the critical role of behaviors in healthcare settings.
How can behavioral wellness strategies enhance health outcomes?
Integrating behavioral wellness strategies into primary care addresses psychological and social factors that influence wellness-related behaviors, thereby improving health outcomes.
What impact did the COVID-19 pandemic have on patient engagement?
The COVID-19 pandemic accelerated the adoption of digital health applications, evidenced by a 30% increase in medical app downloads, indicating a shift towards more engaged care.
How much can adherence to treatment plans improve recovery rates?
Adherence to treatment plans can boost recovery rates by as much as 50%, emphasizing the importance of fostering positive behaviors among patients.
What is the projected demand for Board Certified Behavior Analysts (BCBAs)?
The demand for Board Certified Behavior Analysts (BCBAs) is projected to increase by 25% by 2026, highlighting the growing focus on behavior in medical environments.
Why is transparent communication important in healthcare?
Transparent communication between patients and healthcare providers is vital for improving health outcomes, as emphasized by healthcare professionals.
How does patient engagement data support the importance of engagement tools?
With over 470,000 clients using Updox daily for interaction and communication, and a database containing patient engagement data for 150 million individuals, the significance of engagement tools in enhancing medical outcomes is evident.
Our expert recruitment strategies and AI-driven sourcing ensure that you receive top-notch candidates quickly, without compromising on quality. Whether you’re looking for BCBAs, Clinical Directors, or RBTs, we’ve got you covered.