September 26, 2025

The article titled "10 Essential ABA Billing Codes Every BCBA Must Know" underscores the critical importance of mastering specific billing codes that are essential for Board Certified Behavior Analysts (BCBAs). Understanding these codes is vital for ensuring accurate invoicing and reimbursement for services rendered. While the content of the article is not provided, the title indicates that it will detail key ABA billing codes foundational for effective billing practices. These practices are indispensable for maintaining the financial health of ABA therapy practices.
The landscape of Applied Behavior Analysis (ABA) therapy is evolving rapidly, with the demand for Board Certified Behavior Analysts (BCBAs) expected to surge in the coming years. As this field expands, understanding the intricacies of ABA billing codes becomes paramount for ensuring accurate invoicing and maximizing revenue. However, with frequent updates and complexities in coding practices, how can BCBAs navigate these challenges effectively while enhancing their billing processes?
This article delves into ten essential ABA billing codes that every BCBA must know, providing insights and strategies to streamline billing practices and improve financial outcomes in ABA therapy.
The demand for Board Certified Behavior Analysts (BCBAs) is projected to grow by an impressive 22% to 23% over the next decade, highlighting the robust trajectory of Applied Behavior Analysis therapy as an effective intervention. In this rapidly evolving job market, Hire ABA stands out by linking BCBAs with top job prospects, streamlining the hiring process to ensure that qualified professionals can effortlessly find roles that align with their expertise and career aspirations.
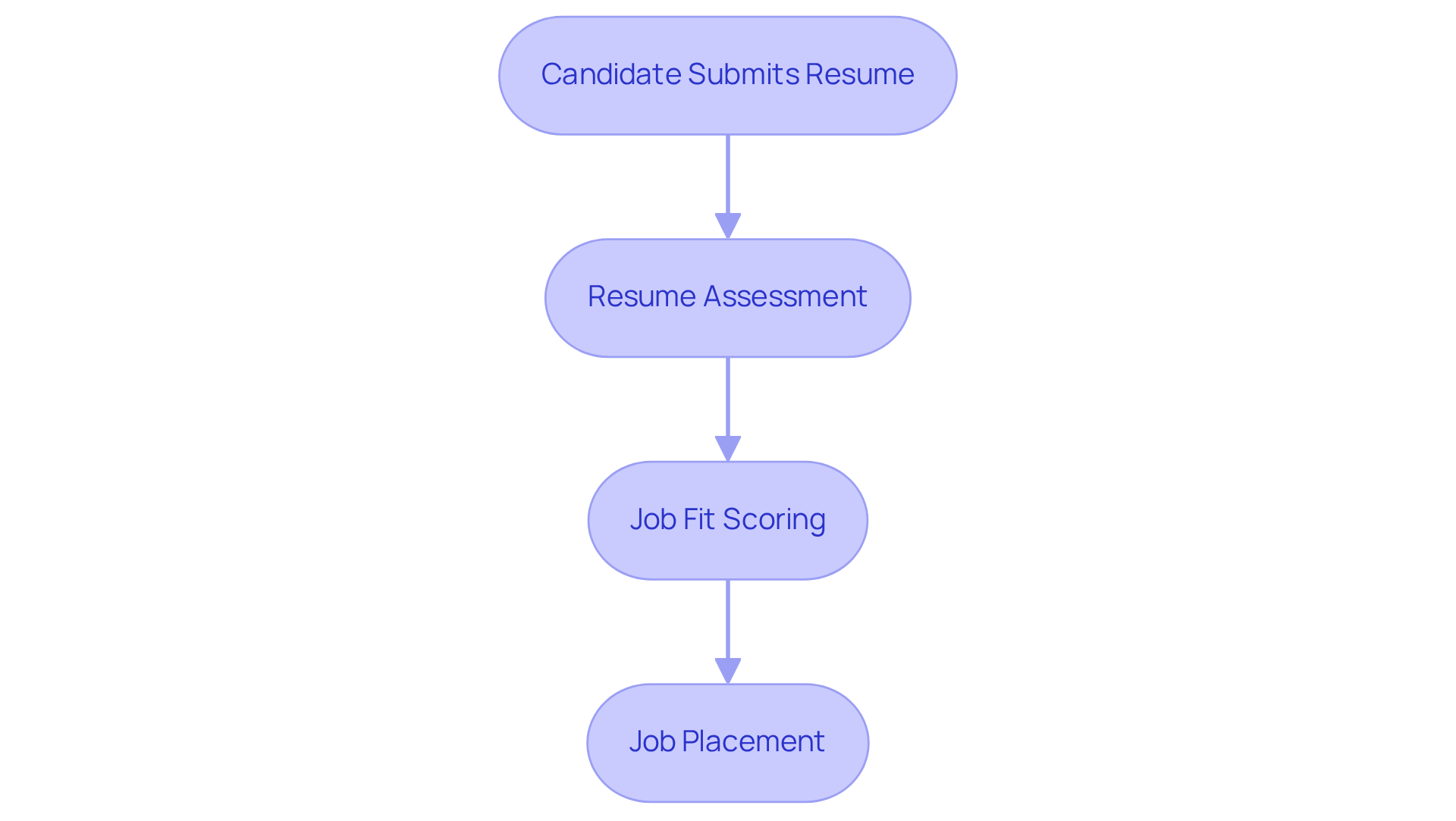
Our personalized resume assessments empower candidates to submit their resumes for evaluation. Our team meticulously assesses their experience and career goals, utilizing advanced job fit scoring to identify opportunities that match their skills, preferences, and desired locations. Are you facing challenges in your current hiring process? Hire ABA prioritizes a supportive and efficient experience, significantly enhancing the job search for candidates in ABA therapy.
This platform not only empowers professionals to advance their careers but also promises job security and competitive salaries, often exceeding average earnings in various professions. Take action today and explore how Hire ABA can transform your career in this promising field.
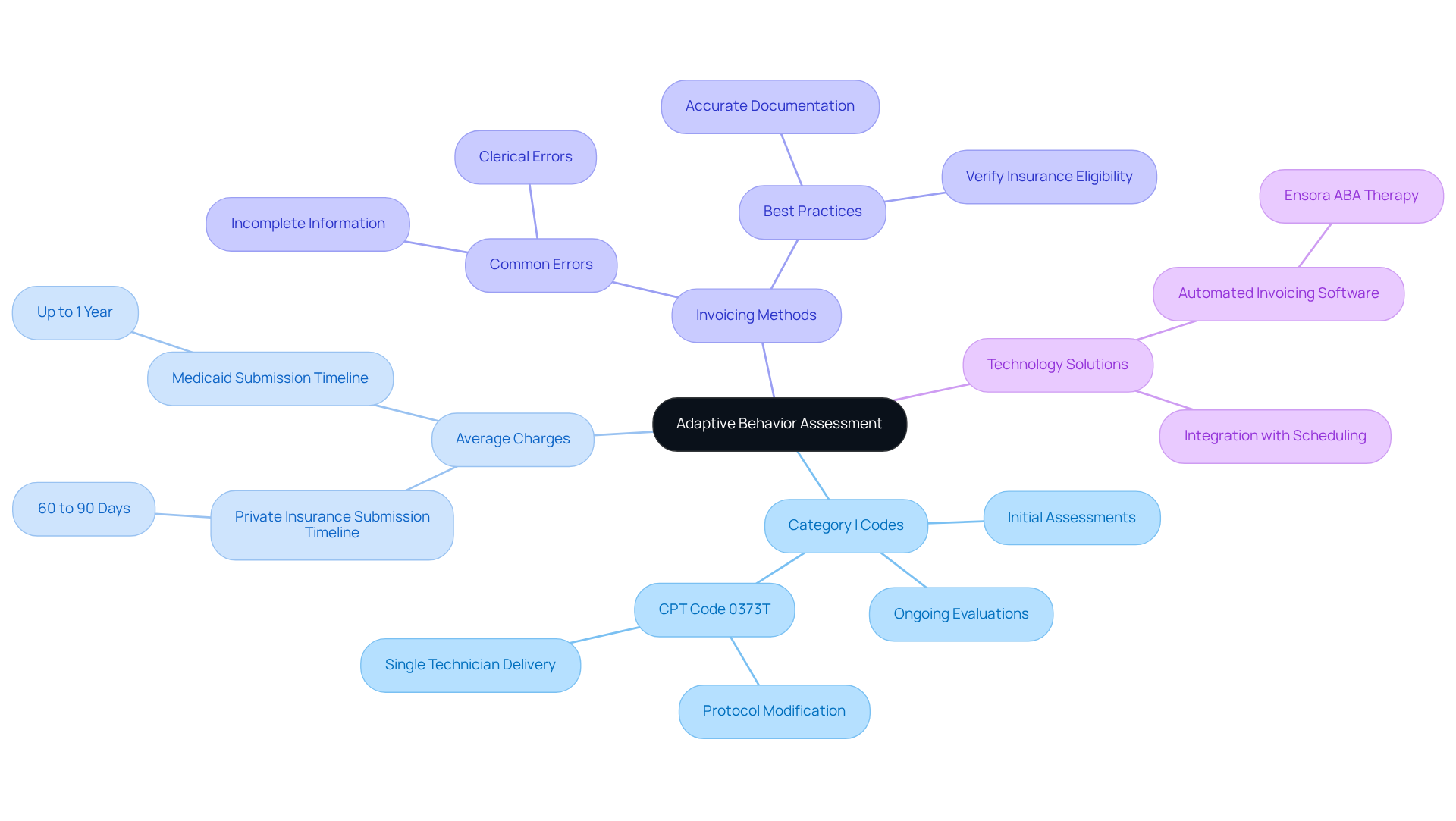
Adaptive Behavior Assessment is a critical process that evaluates a client's behavior to determine the necessity for ABA billing codes. Familiarity with Category I codes is essential for precise invoicing in this context. The ABA billing codes not only aid the invoicing process but also play an essential role in recording client progress and validating treatment plans. Key Category I codes, which include ABA billing codes for initial assessments and ongoing evaluations, are crucial for establishing a comprehensive treatment approach.
The average charges for adaptive behavior evaluations can differ significantly. Comprehending these rates is crucial for establishing competitive pricing and ensuring financial sustainability. For instance, most private insurance providers require that requests be submitted within 60 to 90 days from the date of service, whereas Medicaid permits up to one calendar year to file requests. Effective invoicing methods demand meticulous attention to detail, including verifying client insurance eligibility and ensuring accurate documentation using ABA billing codes. Common pitfalls, such as clerical errors or incomplete information, can lead to claim denials, significantly impacting revenue.
To enhance invoicing efficiency, behavior analysts should consider adopting automated invoicing software, such as Ensora ABA Therapy, which integrates with scheduling and documentation processes. This technology can streamline operations, reduce errors, and enhance overall financial health. Furthermore, remaining aware of the latest modifications to ABA billing codes is essential, as frequent changes can complicate the financial landscape. By implementing these best practices, behavior analysts can ensure they are effectively utilizing Category I codes to support their invoicing processes and enhance client care.
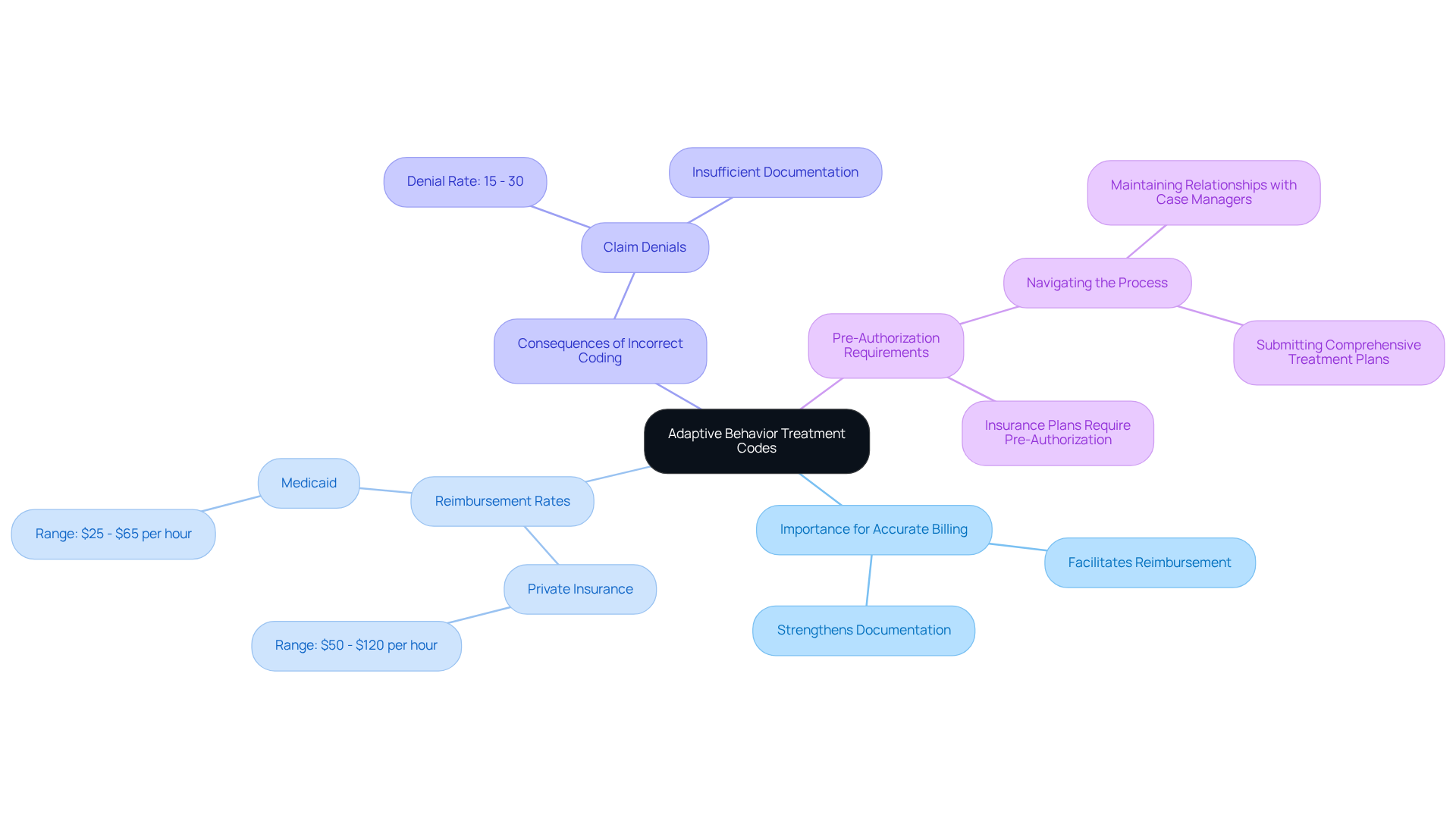
Adaptive Behavior Treatment codes, also known as ABA billing codes, are pivotal for the accurate billing of therapeutic services provided to clients. These Category I codes encompass a variety of treatment modalities, including both individual and group therapy sessions. Behavior analysts must utilize the correct codes to ensure that the services rendered are accurately documented. This not only facilitates reimbursement but also strengthens the documentation of treatment efficacy and client outcomes.
With average reimbursement rates for ABA therapy sessions ranging from $50 to $120 per hour for private insurance and $25 to $65 for Medicaid, a thorough understanding of ABA billing codes is essential for maximizing revenue. Billing specialists emphasize that precise coding is foundational for successful claims, as insufficient documentation is a leading cause of claim denials, which can range from 15% to 30%.
Furthermore, many insurance plans require pre-authorization before ABA services commence, making it essential for behavior analysts to navigate this process effectively. Consequently, behavior analysts should focus on mastering ABA billing codes to improve their payment practices and the overall quality of care delivered.
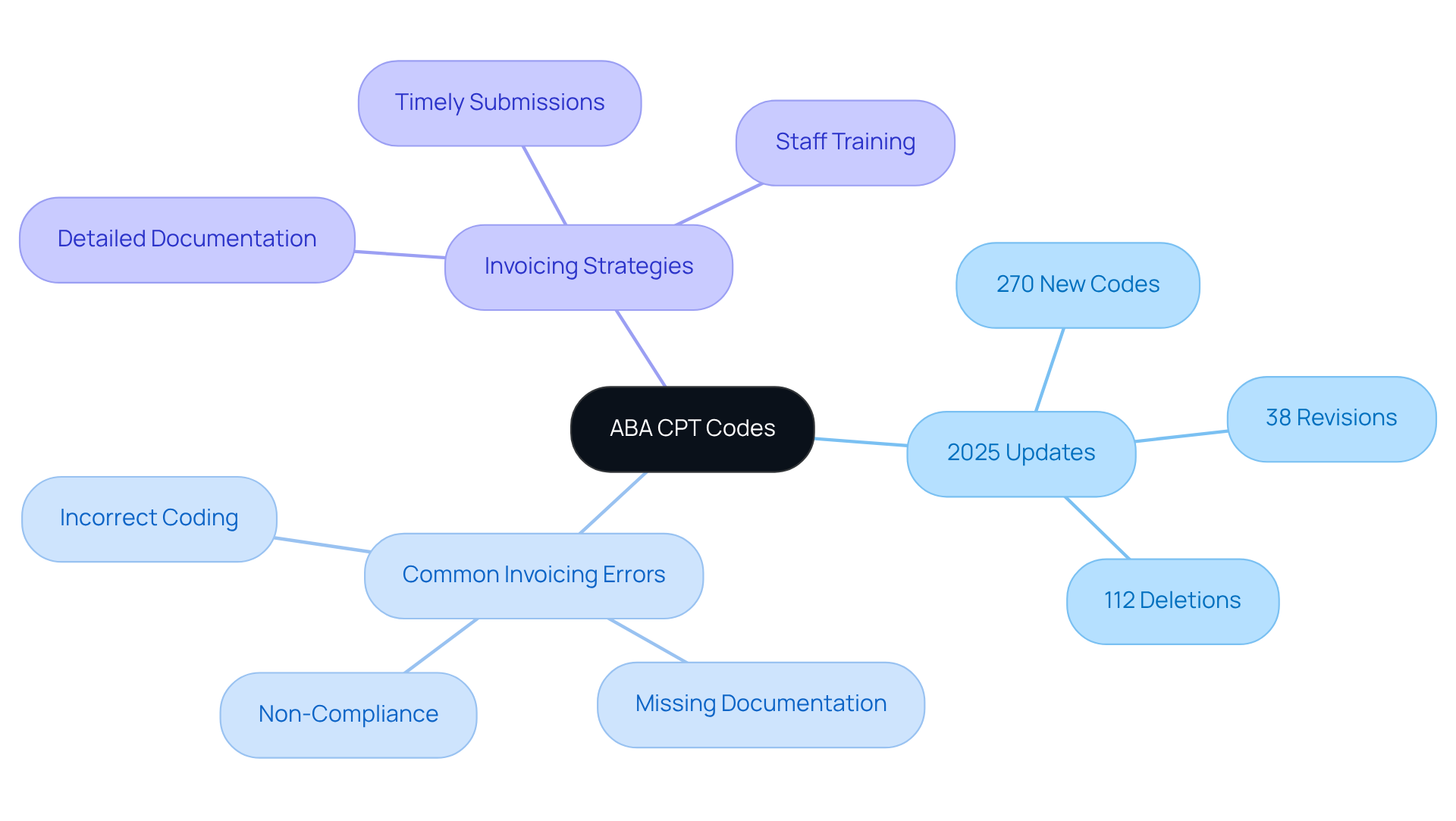
Current Procedural Terminology (CPT) codes are vital tools for Board Certified Behavior Analysts (BCBAs), offering a standardized language to articulate medical, surgical, and diagnostic services. Mastery of ABA billing codes is crucial for BCBAs to ensure accurate invoicing and efficient processing of requests. The 2025 CPT update brings significant changes:
This makes it imperative for behavior analysts to remain informed.
Regularly reviewing these codes helps BCBAs avoid common invoicing errors, such as:
Such mistakes can lead to request denials and financial repercussions. Experts emphasize that a thorough understanding of ABA billing codes directly impacts invoicing accuracy, thereby supporting the financial health of ABA practices.
Implementing effective invoicing strategies—such as detailed documentation, timely request submissions, and ongoing staff training on coding protocols—can significantly enhance reimbursement rates. By prioritizing CPT code comprehension and utilizing resources like TherapyPM, which offers training modules and automated updates on coding changes, behavior analysts can navigate the complexities of invoicing with confidence. This ensures compliance with insurance standards and bolsters their practice's revenue cycle.
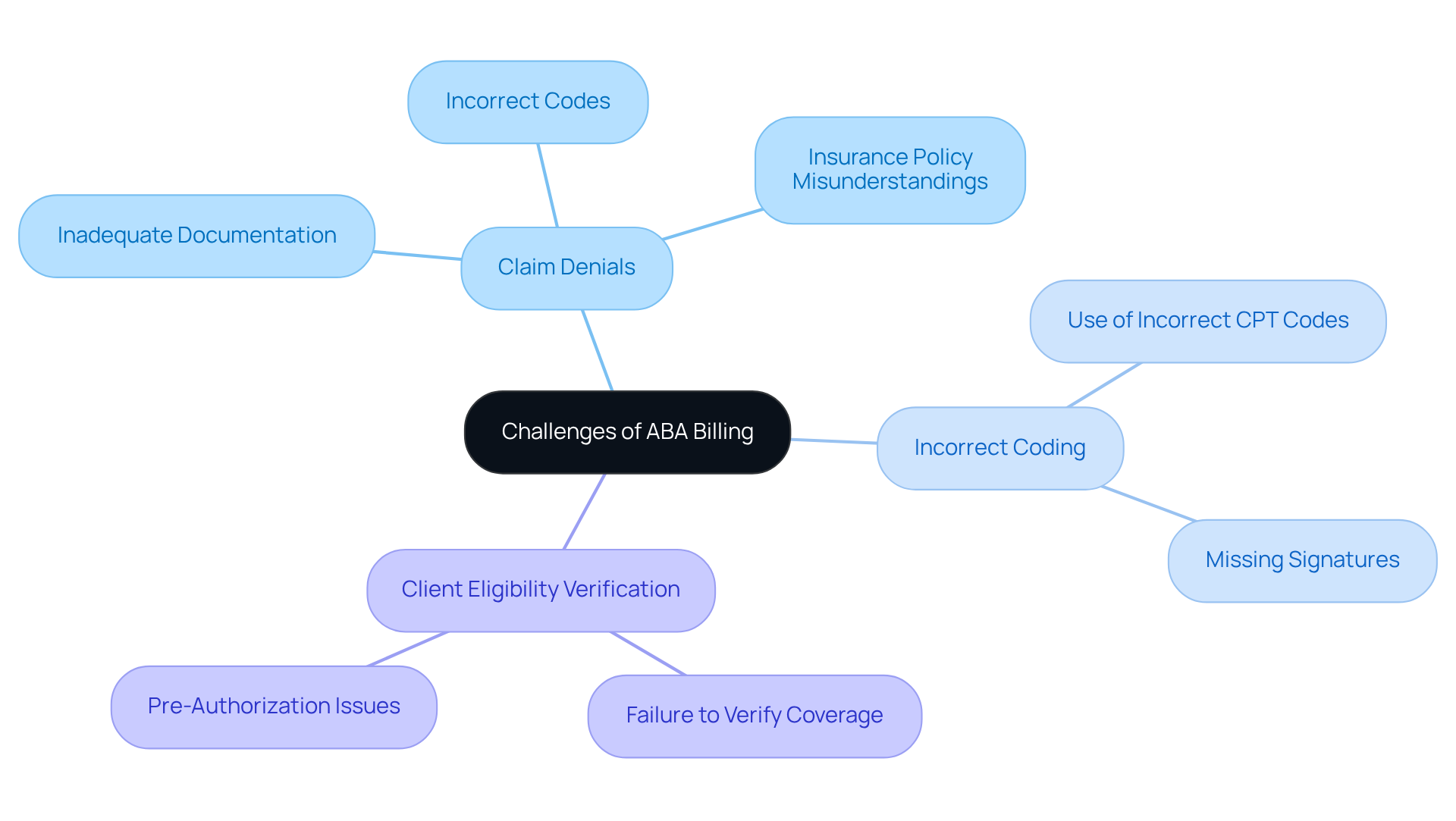
ABA billing presents notable challenges, including claim denials, incorrect coding, and issues with client eligibility verification. Behavior analysts must proactively identify these challenges to minimize their impact on revenue. Common issues include:
By remaining informed and implementing best practices, behavior analysts can navigate these challenges effectively.
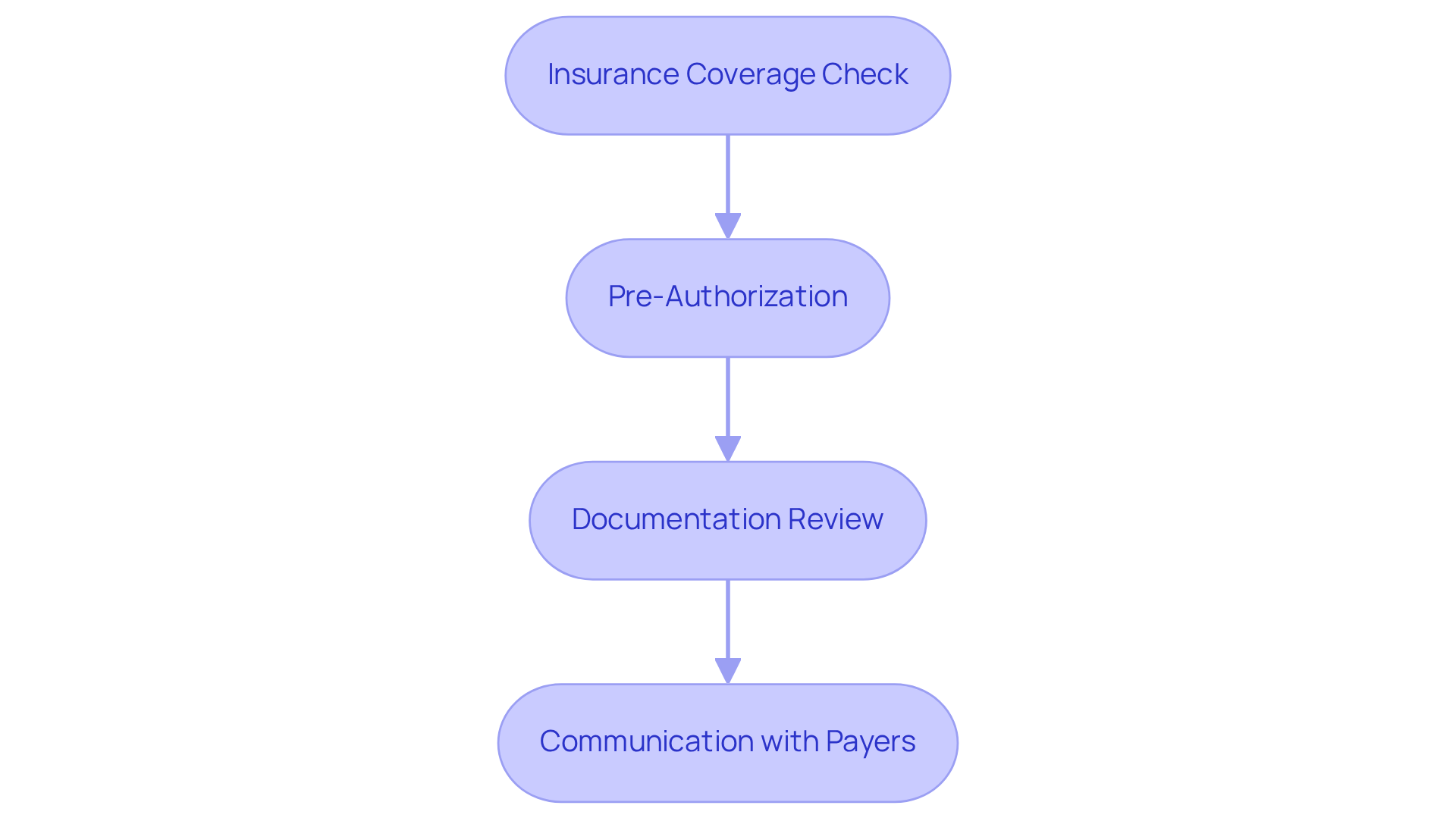
Before submitting requests, it is vital for Board Certified Behavior Analysts (BCBAs) to confirm client eligibility for ABA billing codes. This process entails verifying that the client's insurance covers the specific services rendered and that the appropriate ABA billing codes are used, ensuring all necessary criteria are met. Failing to confirm eligibility for ABA billing codes can lead to denials and postponed payments, which significantly impacts the financial well-being of the practice. Monthly expenses for ABA therapy can range from $4,800 to over $20,000, underscoring the financial stakes involved in this process. A systematic approach to eligibility verification should include the following steps:
Experts stress that effective eligibility verification with ABA billing codes can significantly improve approval rates. As noted by industry professionals, 'Authorization drives everything in ABA billing codes,' highlighting the critical nature of this step. Additionally, Rajgopal advises, 'Make sure your eligibility verification process aligns with the ABA billing codes,' reinforcing the importance of diligence in this area. By establishing a comprehensive verification method, behavior analysts can reduce the risk of denial of requests, which frequently stem from the intricacies of financial practices and the absence of consistent guidelines, facilitating a more seamless financial experience.
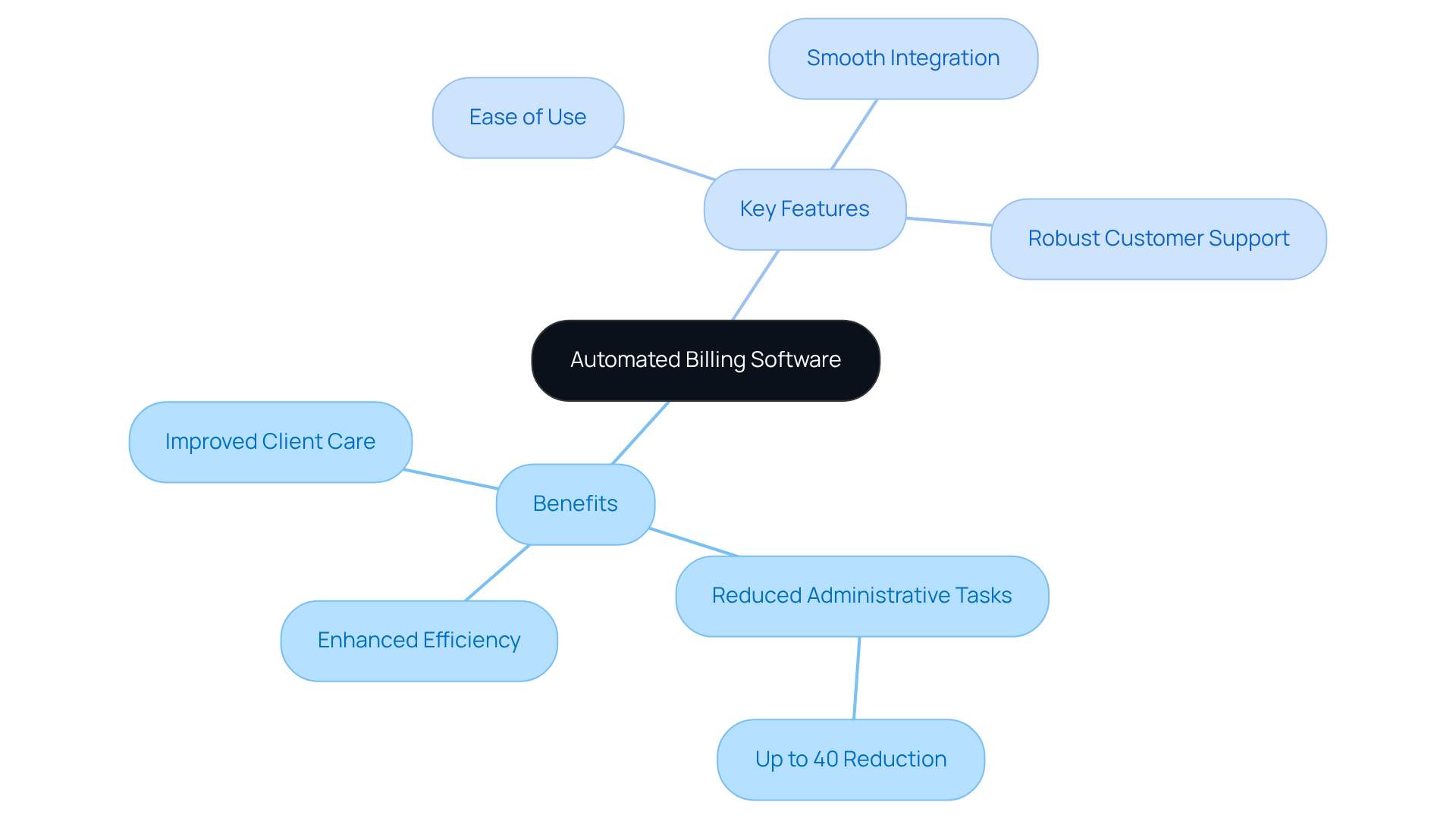
Automated invoicing software significantly enhances the efficiency of payment processes related to ABA billing codes, streamlining essential tasks such as claim submission, payment tracking, and client record management. By automating these functions, Board Certified Behavior Analysts can reduce mistakes, allowing them to dedicate more time to client care and ultimately enhancing service delivery. Did you know that ABA EMR platforms can reduce administrative tasks by up to 40%? This statistic underscores the potential for clinicians to focus more on direct patient care.
When assessing invoicing software, behavior analysts should prioritize features such as:
As highlighted by ABASmart, an ABA EMR system is designed with ease of use in mind, ensuring compliance with payer and legal standards, including ABA billing codes. Furthermore, behavior analysts should consider examining case studies, such as those on optimizing ABA documentation methods, to understand the practical advantages of automated invoicing software. To maximize the benefits of these tools, behavior analysts are encouraged to evaluate their current billing processes against the features offered by automated software.
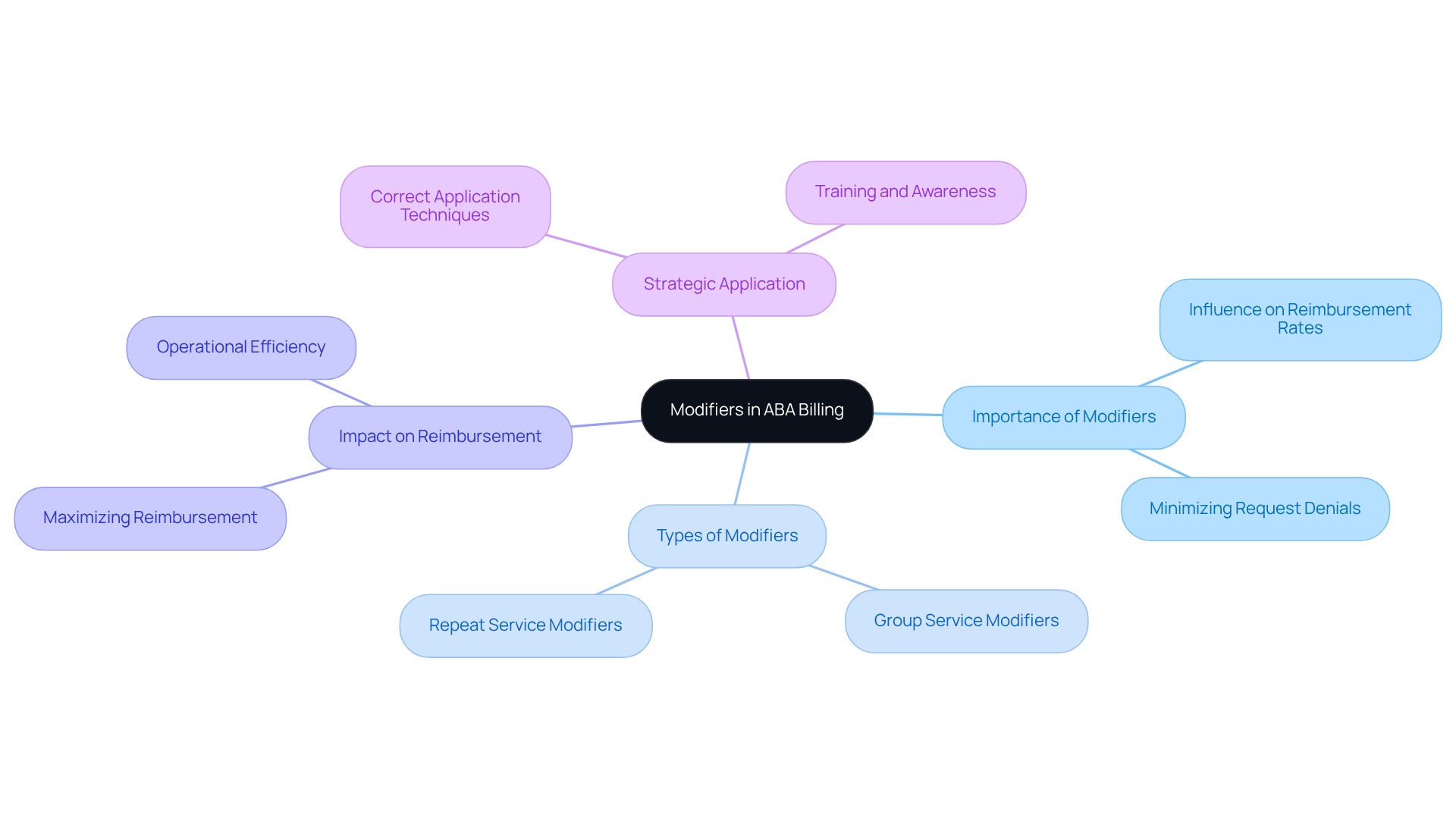
Modifiers are essential codes that provide critical detail about the services rendered, significantly influencing reimbursement rates. Understanding how to utilize modifiers effectively is crucial for behavior analysts to ensure accurate submissions. For instance, modifiers can indicate whether a service was delivered in a group setting or if it was a repeat service. Correct application of these modifiers not only maximizes reimbursement but also minimizes the risk of request denials. Are you aware of how these nuances can impact your practice? Properly leveraging modifiers is a strategic move that can enhance your operational efficiency.
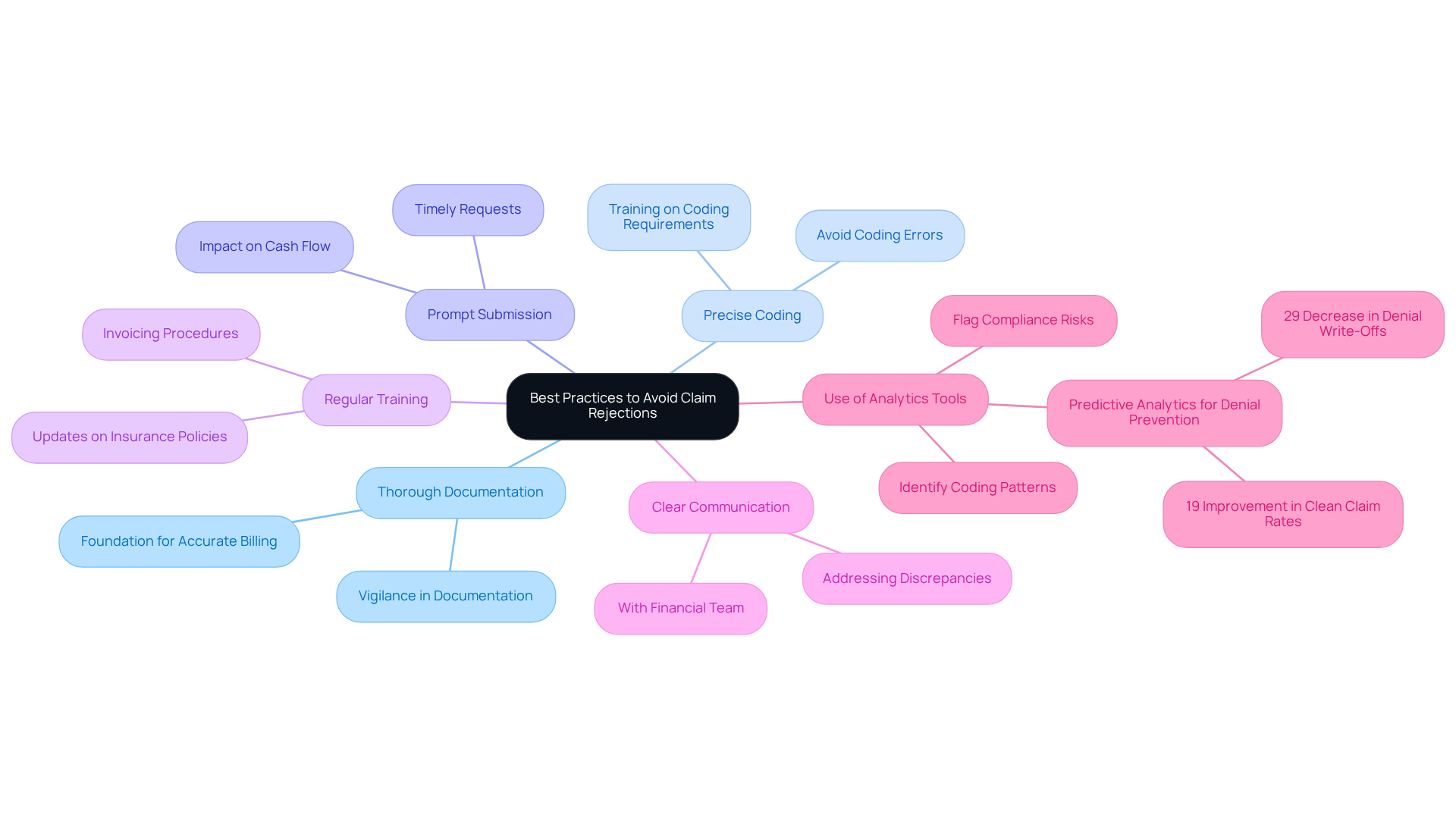
To reduce denial of requests, Board Certified Behavior Analysts (BCBAs) should adopt several best practices. Startlingly, insurers reported receiving 425 million requests in 2023, with an average denial rate of 20%. This statistic underscores the urgent need for vigilance in documentation and coding.
First and foremost, thorough documentation of services rendered is essential, as it serves as the foundation for accurate billing. Coupled with this, precise coding is crucial; errors in coding can lead to significant delays and denials, further complicating the reimbursement process.
Prompt submission of requests is another essential aspect. Delays can exacerbate the risk of rejections, impacting cash flow and operational efficiency. Regular training sessions on invoicing procedures can keep staff updated about the latest insurance policies and coding requirements, further decreasing the chances of mistakes. For instance, organizations that implemented predictive analytics for denial prevention experienced a 29% decrease in denial write-offs and a 19% improvement in clean claim rates, according to Plutus Health.
Establishing clear communication channels with the financial team is also vital. This ensures that any discrepancies or issues are promptly addressed, facilitating a smoother billing process. Analytics tools can flag potential compliance risks and identify coding patterns with a higher likelihood of denials, providing actionable insights for behavior analysts. By promoting a cooperative atmosphere, behavior analysts can enhance the precision of their submissions and boost overall success rates.
As the landscape of ABA invoicing continues to evolve, staying proactive in these practices will be key to navigating the complexities of insurance claims effectively.
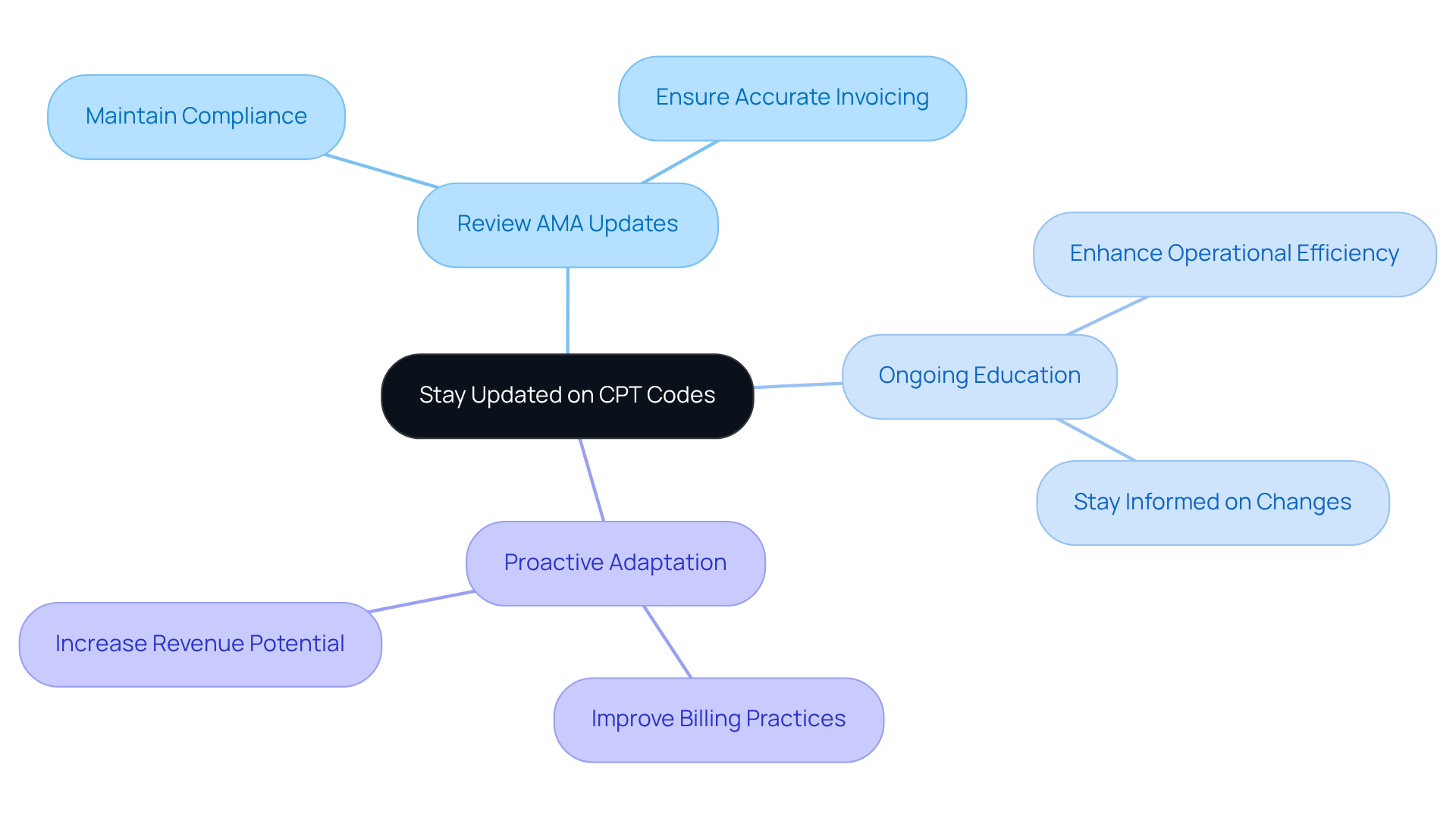
The terrain of CPT codes is in a constant state of flux, necessitating that behavior analysts remain vigilant regarding any changes that could affect their payment procedures. Regularly reviewing updates from the American Medical Association (AMA) and participating in ongoing educational opportunities are vital strategies for behavior analysts to maintain compliance and ensure accurate invoicing. By proactively adapting to modifications in CPT codes, BCBAs can significantly enhance their billing practices and boost their overall operational efficiency.
Understanding and mastering the essential ABA billing codes is crucial for Board Certified Behavior Analysts (BCBAs) to navigate the complexities of the billing landscape effectively. With the projected growth in demand for BCBAs, being well-versed in these codes not only enhances invoicing accuracy but also plays a pivotal role in ensuring the financial health of ABA practices.
This article delves into the significance of various billing codes, including:
Key insights highlight the necessity of:
By adopting best practices and staying updated on the latest changes in billing codes, behavior analysts can significantly reduce claim denials and improve their overall operational efficiency.
As the field of ABA therapy continues to evolve, staying informed and proactive in billing practices is essential. BCBAs are encouraged to leverage available resources, such as automated invoicing systems and ongoing education, to enhance their billing processes. Embracing these strategies not only supports individual practices but also contributes to the overall advancement of the profession, ensuring that clients receive the quality care they deserve while securing the financial sustainability of ABA services.
What is Hire ABA and how does it benefit BCBAs?
Hire ABA is a platform that connects Board Certified Behavior Analysts (BCBAs) with job opportunities in Applied Behavior Analysis therapy. It streamlines the hiring process, helping qualified professionals find roles that match their expertise and career goals.
How does Hire ABA assist candidates in their job search?
Hire ABA offers personalized resume assessments to evaluate candidates' experience and career aspirations. It uses advanced job fit scoring to identify suitable job opportunities based on candidates' skills, preferences, and desired locations.
What is the projected demand for BCBAs in the coming years?
The demand for BCBAs is projected to grow by 22% to 23% over the next decade, indicating a strong need for professionals in Applied Behavior Analysis therapy.
What are Category I codes in the context of ABA therapy?
Category I codes are billing codes used in Adaptive Behavior Assessment and Treatment. They are essential for accurate invoicing, recording client progress, and validating treatment plans in ABA therapy.
Why is understanding Category I codes important for behavior analysts?
Understanding Category I codes is crucial for behavior analysts to ensure precise invoicing, maximize revenue, and avoid claim denials due to insufficient documentation.
What are the average reimbursement rates for ABA therapy sessions?
Average reimbursement rates for ABA therapy sessions range from $50 to $120 per hour for private insurance and $25 to $65 for Medicaid.
What common pitfalls should behavior analysts avoid in the billing process?
Common pitfalls include clerical errors, incomplete information, and failing to verify client insurance eligibility, which can lead to claim denials and negatively impact revenue.
How can behavior analysts improve their invoicing efficiency?
Behavior analysts can enhance invoicing efficiency by adopting automated invoicing software, such as Ensora ABA Therapy, which integrates with scheduling and documentation processes to reduce errors and streamline operations.
What should behavior analysts be aware of regarding ABA billing codes?
Behavior analysts should stay informed about the latest modifications to ABA billing codes, as frequent changes can complicate the financial landscape and affect their billing practices.
Our expert recruitment strategies and AI-driven sourcing ensure that you receive top-notch candidates quickly, without compromising on quality. Whether you’re looking for BCBAs, Clinical Directors, or RBTs, we’ve got you covered.